Third Party Administrator(TPA) Services in Manassas
When you're running a business, taking care of your team’s health isn’t just the right thing to do—it’s part of keeping your company running smoothly. At Altmed Medical Center, we help take that load off your plate by offering Third-Party Administrator (TPA) services designed for local employers right here in Manassas, VA.
From trucking companies near Route 234 to small businesses by the Manassas Mall, we support your team’s health needs so you can stay focused on running your business.
What Is a TPA and Why Does It Matter?
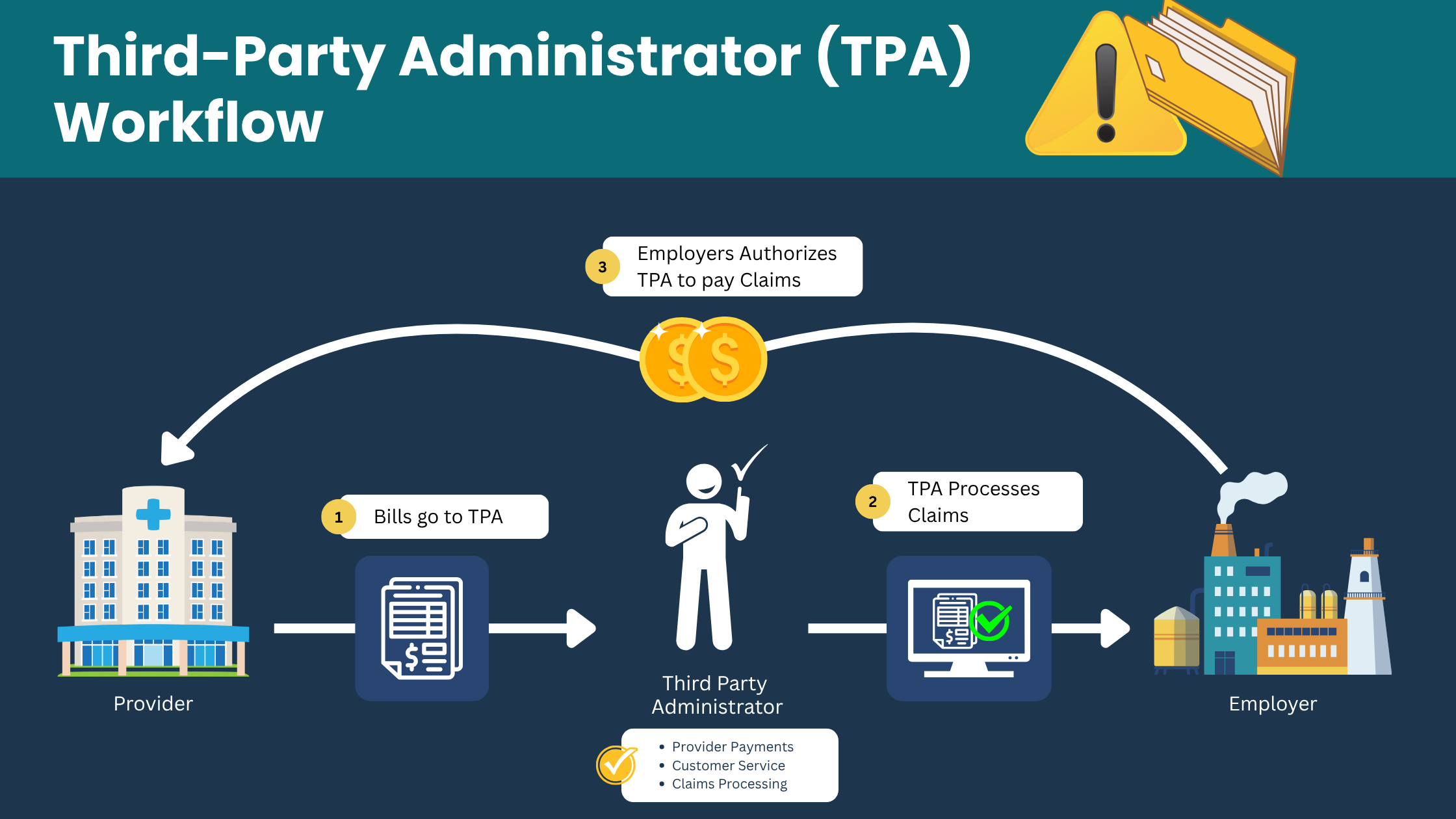
A Third-Party Administrator (TPA) helps employers manage health and safety programs in the workplace—especially things like drug testing, physicals, and regulatory paperwork.
While some TPAs deal with insurance, that’s not what we do. At Altmed, our focus is squarely on occupational health. We’re here to make sure your team meets all the right requirements—without creating more work for you.
Who Uses TPA Services?
A wide range of businesses in and around Manassas count on TPA services to stay compliant and protect their staff. You might benefit too if you're in one of these industries:
- Trucking & Transportation: DOT compliance is serious business. We handle driver drug testing and physicals to help you stay on track.
- Construction & Contracting: Make sure your crews are fit and meet safety guidelines.
- Government Contractors: From background checks to health screenings, we help meet federal and local requirements.
- Staffing Agencies: Need to get temporary hires cleared fast? We’ve got you covered.
- Local Businesses: Even with just a few employees, it’s easy to fall behind on health compliance. We help you stay ahead.
We work with companies throughout Manassas, Bristow, Nokesville, and along Prince William Parkway.
TPA Services We Offer at Altmed
We provide everything you need to manage employee health programs without hassle. Here’s what’s included:
- DOT & Non-DOT Drug Testing
We’ll help you meet federal and company-specific testing needs with speed and accuracy. - Pre-Employment Physicals
Make sure your new hires are ready and able to do the job before they start. - Random Drug Testing Program Management
We’ll organize and manage your random testing pool so it’s done right and on time. - Post-Accident & Return-to-Duty Testing
Ensure your workplace stays safe and compliant after an incident or employee leave. - Regulatory Paperwork & Compliance Support
Our team handles the paperwork, so you don’t have to worry about forms, deadlines, or missing something important.
Need quality care fast? Our team is here for all your primary care and urgent care needs. Walk-ins welcome and same-day appointments available. Call (703)-361-4357 OR
Make an AppointmentHow It Works (It's Easy)
Partnering with us is simple and stress-free. Here's what the process typically looks like:
- Send your employees in – Walk-ins are welcome, and we’re centrally located in Manassas.
- We do the testing – Fast, professional service with minimal wait times.
- You get results – We’ll send you secure, timely results.
- You stay compliant – We track what’s needed and help you stay ahead of regulations.
Employers appreciate how fast and smooth the process is—no chasing labs, no lost paperwork, no confusion.
Why Businesses Choose Altmed for TPA Services
We're more than just a clinic. We’re a local partner who understands what it's like to run a business in this community
- Walk-In Friendly: No need to book ahead. Send employees as needed.
- Great Location: We’re close to Liberia Ave and I-66, making it easy for teams from across Prince William County to reach us.
- Budget-Friendly Options: Our pricing is fair, transparent, and can be tailored to fit your business size.
- DOT & FMCSA Expertise: We stay up-to-date on current regulations so you don’t have to.
Real Example: A Local Trucking Company
Let’s say you run a small trucking company near Manassas Regional Airport. You’ve got a handful of drivers and a lot on your plate. Keeping up with DOT testing requirements and physicals isn’t easy.
That’s where we step in. You send your drivers our way—we handle the drug tests, complete the paperwork, and get everything back to you quickly. No chasing labs, no compliance headaches. Just one less thing for you to worry about.
Ready to Get Started?
If you're a business owner, HR manager, or safety officer looking for a trusted TPA partner, we’re here to help.
We’ll take the stress out of drug testing, physicals, and workplace compliance—so you can focus on what matters most: your people and your business.
Need care today? We’ve got you covered — walk-ins welcome and same-day appointments available at Altmed Medical Center.
Call (703) 361-4357 or
